Uncovering antimicrobial resistance in unusual places
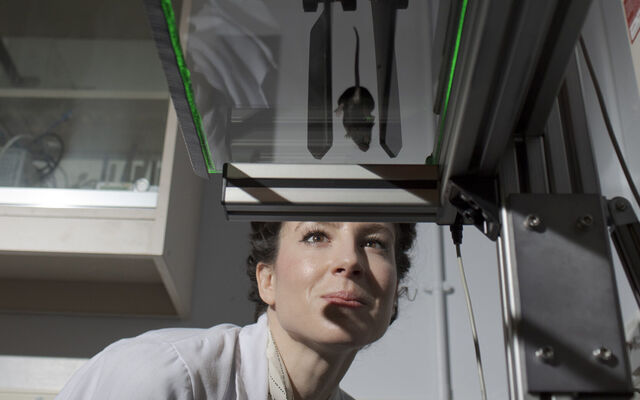
Dr Jordan Sealey is working to gain insights into antimicrobial resistance from zoo and animal studies.
Antimicrobial resistance (AMR) is a pressing global concern, threatening our ability to combat once-treatable infections.
Research by Dr Jordan Sealey, our former PhD student, has explored AMR in diverse contexts, from humans to dogs, cattle, and zoo animals, shedding light on potential risks and prevention strategies.

"Bacteria are everywhere," Jordan explains. "Some are considered as 'good' and others are considered as 'bad' bacteria. Everyday interactions between humans, animals, and the environment allow for the sharing of bacteria, and this includes resistant bacteria."
"Studies have shown that, in hospitals, resistant bacteria can spread within settings between patients and staff. Similarly, in veterinary practices and farms, resistance can transfer between staff and animals."
"Rates of resistant infections are increasing, and one way we can tackle this threat is to understand where it is coming from and implement strategies to prevent this from happening."
After an academic journey that began in zoology, and a master’s studying infectious diseases and disease vectors, Jordan joined our National PhD Training Programme in AMR Research, based at the University of Bristol, focusing on the transmission of bacterial resistance between humans, animals, and the environment.


Dogs as intermediaries in bacterial transmission
As part of the OH-STAR project (One Health Surveillance for Tracking Antibiotic Resistance), researchers at the University of Bristol examined resistant E. coli strains in humans and dairy cattle in southwest England.
One Health is an approach that recognizes that the health of people is closely connected to the health of animals and our shared environment.
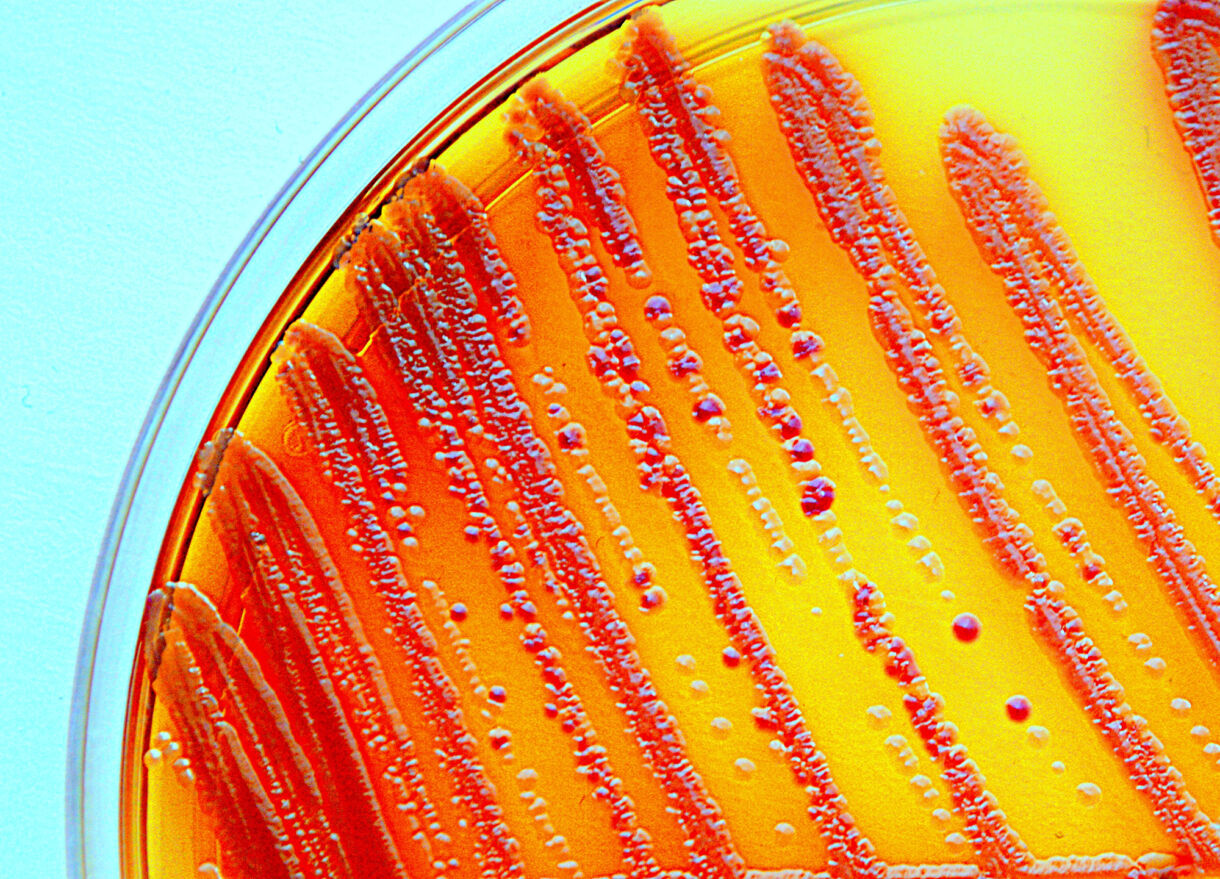
E. coli are important gut commensal bacteria, but are also responsible for various infections, including urinary tract and bloodstream infections. The study used genetic analysis to investigate bacterial sharing between cattle and humans, revealing limited evidence of transmission.

Dogs live very closely with people, and that closeness can make it easy for resistant bacteria to spread.

With the OH-STAR project as a springboard, Jordan added another one-health compartment, dogs, into the study. Dogs, living closely with humans, could offer insights into bacterial transmission due to their shared environments.
She homed in on two crucial classes of antibiotics: third-generation cephalosporins and fluoroquinolones. These antibiotics, classified as 'highest priority critically important' by the World Health Organization, are often considered the last line of defence against complicated infections.
Jordan designed a comprehensive study that involved recruiting 600 dog owners within the region to complete a survey about their dog and provide a faecal samples.
Samples were sent to the lab to obtain commensal gut E.coli for microbiological and genetic analysis. She used whole-genome sequencing, a process for understanding the entirety of the DNA sequence of an organism, revealing all the genetic information that makes it unique.
Her research revealed distinct E. coli strains in rural dogs compared to urban dogs, with evidence of resistant bacteria being shared between dogs living in rural environments and cattle, and between humans and dogs.
Furthermore, the statistical analysis from the survey data showed a strong association between raw feeding and dogs carrying resistance to both highest priority critically important antibiotics. Importantly, this reflects results found in other similar studies.
Urban river swimming was also found to be associated with third-generation cephalosporin resistance.

Antibiotic resistance in zoo animals
Similarly, zoos are environments that house multiple species for humans to come close to, and potentially share bacteria. But they have been largely understudied in relation to AMR.
Jordan’s study, which concentrated exclusively on captive animals living within a city and the study region, Bristol Zoo, used whole genome sequencing and phylogenetic analysis to discover resistant E. coli
across the different species.
Phylogenetic analysis is a method of studying the evolutionary history of certain species by examining their ancestry and genetic similarities.
Her research showed high levels of antibiotic resistance within the animals at the zoo, with over 50 per cent of samples showing resistance. This contrasted with resistance levels of around 10 per cent in cattle and dogs within the same region.
The reason for this may owe to the fact that many zoo animals are endangered or highly-prized, and therefore their health is monitored very closely, with vets on-hand to administer drugs and treatments.
They found four different types of resistance mechanisms in the zoo to amoxicillin-clavulanate, which, when they investigated further, turned out to be the most frequently used antibiotic in the zoo.
Over 50%
of zoo samples showed antibiotic resistance
Prevention is better than a cure. If we know where resistance comes from we can implement ways to stop it from spreading in the first place, reducing resistance and preventing infection.
Jordan’s research also uncovered resistance strains in zoo animals that had not been previously identified in dogs, cattle, or humans within the same geographical area.
Significantly, the study highlighted evidence of circulation of antibiotic resistance between different enclosures and animal species in the zoo, despite them not being in direct physical contact.
Several possibilities that could have contributed to this include pests, run-off, and human movement between enclosures. Further studies are needed to determine cause and implement prevention strategies, and to investigate whether people working in the zoo share bacteria in common.

What this means for our communities
Jordan’s research has far-reaching implications to human and animal health, emphasising the need to reduce antibiotic use, implement good hygiene practices, and consider policy changes to reduce resistance transmission in a variety of environments, including in the veterinary industry and in raw food manufacturing.
Her work underscores the role of research in preventing antibiotic resistance and highlights the importance of early intervention.
These studies provide an understanding of the potential resistance threat and how we can reduce it. Follow-up studies are also important to know the impact of any policy or technique that’s been implemented. Jordan Sealey

Foundation funding: Fuelling Scientific Discoveries
Funding plays a critical role in conducting studies like this. It enables researchers like Jordan to make ground-breaking discoveries by providing stipends (support for basic costs to the researcher), covering lab processing costs, and facilitating conference presentations.
Jordan has published papers in the Journal of Antimicrobial Chemotherapy, One Health, and the Journal of Applied Microbiology:
Jordan has presented her data at the annual Medical Research Foundation AMR conferences and international conferences like the American Society for Microbiology (ASM), the European Society of Clinical Microbiology and Infectious Diseases (ECCMID) and the International Society for Infectious Diseases (ISID), where she shared her findings with the global scientific community.
What next?
Looking ahead, Jordan is embarking on a project in collaboration with the Welsh government to study resistance on Welsh farms.

Her long-term interest lies in understanding the transmission of resistant infections between humans, animals, and the environment to reveal pathways of bacterial sharing and develop control strategies.
Dr Jordan Sealey's research emphasises the importance of carrying out holistic studies that combine resistance data, risk analysis, and phylogenetics. Early intervention, responsible antibiotic use, and rigorous hygiene practices are essential in addressing this global challenge.
Help fund more research like this
Donate to support ground-breaking research into areas of unmet need
Support usWhile this page was originally published as a standalone piece, Dr Jordan Sealey's research features in our 2025 Impact Report.
Help fund more research like this
Donate to support ground-breaking research into areas of unmet need.
Donate